Stress Incontinence
Stress incontinence is very familiar to most women. It is involuntary urine loss with activity that is caused by an increase in abdominal pressure, such as with coughing, sneezing or running. This is due to the inability of the urethra (the tube through which urine exits the body) to maintain a higher pressure than the bladder during these periods of exertion. The urethra is a muscular tube where the walls are normally touching (like a collapsed fire hose) unless we are urinating or something is placed in it. This allows the urethra to act like a shut off valve in that the pressure in the urethra is higher than the pressure in the bladder unless we are urinating or incontinent. Factors that contribute to urethra pressure are the muscle tone of the urethra muscles themselves, the tone and strength of the pelvic floor muscles (Kegel’s exercises), the thickness of the urethra mucosa (which can be affected by estrogen), and the position of the urethra within the abdominal cavity. The most common cause of stress incontinence is a loss of support of the urethra due to trauma with childbirth but it can also be due to chronic cough, constipation, or a scarred urethra such as with prior surgery. Loss of support allows the urethra to descend below the pelvic floor muscles (and outside the abdominal cavity) when abdominal pressure is raised such as with coughing, sneezing, laughing or just getting up from a chair. During activity the increase in abdominal pressure is applied to the bladder (like squeezing a water balloon) which makes the water want to go out of the urethra (neck of the balloon). Normally the same squeezing force that raises the pressure inside the bladder also compresses (raises the pressure inside) the urethra to compensate and we don’t leak. Think of squeezing an untied water balloon. You can squeeze the balloon all you want and not spill water so long as you squeeze the neck of the balloon closed as well. Unfortunately the same abdominal pressure that squeezes the bladder also forces the urethra downward in people who have lost support. That means the urethra is no longer exposed to the compression that would ordinarily counteract the increase in bladder pressure. The pressure in the urethra is unable to “keep up” with the pressure in the bladder and you leak. For more information, click here.
Treatments
Treatments for stress incontinence are directed toward preventing that pressure imbalance between the bladder and urethra. Physical therapy improves the strength and tone of the pelvic floor muscles which helps compress the urethra shut and stabilize it within the abdominal cavity. Even if we are not consciously squeezing our pelvic floor muscles (Kegel’s) the increased tone from exercise helps improve urethra pressure. Additionally we all have a “guarding reflex” so that we automatically Kegel when we cough or sneeze.
Pelvic Muscle Strengthening
Once you learn how to “Kegel,” you can Kegel anywhere. The trick is finding the right muscles to squeeze. Your doctor or nurse can help make sure you are. After about 6 to 8 weeks, you should notice squeezing the right muscles. Your doctor may refer you to a specially trained physical therapist who will teach you to find and strengthen the sphincter muscles. Learning when to squeeze these muscles can also help stop the bladder spasms that cause urge incontinence that you have fewer leaks and more bladder control. Use the pelvic muscle exercise log included with the Kegel Exercise Tips sheet (Item C) to keep track of your progress. Many women prefer to try the simplest treatment choices first. Kegel exercises strengthen the pelvic muscles and don’t require any equipment. Follow this link to learn more.
Pessaries
A pessary is a vaginal support device made of silicone rubber that pushes against the vaginal side of the urethra and compresses it shut when you exert yourself. It acts as if you put your finger in the vagina and pressed the urethra shut every time you coughed. The benefit is that it is nonsurgical but the downside is you have to put it in, take it out and clean it. Estrogen can be helpful in ladies past the change (menopausal) in that it thickens the urethra mucosa, which makes for a snugger closure. For more information, click here.
Medication and Surgery
A medication called Duloxetine (trade name Cymbalta®) can also be helpful in raising urethra pressure by actually contracting the muscles in the walls of the urethra. The upside is it improves stress incontinence about 60% of the time. The downside is that you must take the medicine indefinitely. Vaginal estrogen helps with stress urinary incontinence by thickening the walls of the urethra so that they close tighter and prevent leaking.
You may have heard of someone’s “bladder being tied up” which refers to a bladder suspension. The two most common such surgeries are the Burch and the MMK. These surgeries stabilize the urethra to prevent the downward motion out of the abdomen by suspending it to the pubic bone. Think of the Golden Gate Bridge. The roadway is the urethra, and the vertical cables suspend it from a structure above. This keeps the urethra in the abdomen and exposed to the same counteracting forces that squeeze the urethra shut when abdominal pressure is raised.
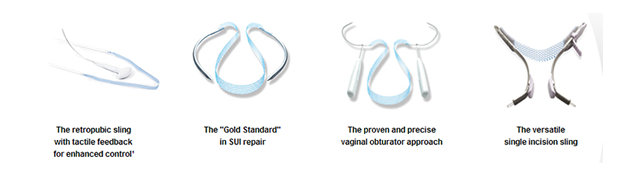
The trend in recent years has been away from these bladder suspensions and toward sub urethral slings click here. The trend in recent years has been away from these bladder suspensions and toward sub urethral slings. This is in part due to the arrival of self securing slings that are easier to perform. Sub urethral slings are actually the oldest incontinence surgeries but they had become less popular with the advent of bladder suspensions as described above. This is because the suspensions were simpler to perform, and could be done through he same incision as a hysterectomy. These surgeries consist of a band of material looped under the urethra and attached to another structure such as the abdominal wall or pelvic floor muscles and connective tissue. A good analogy is a child in a swing set. The child is in the place of the urethra and the swing chain and seat are the sling. The cross bar the swing is hanging from is the abdominal wall. The urethra (child) can only fall as far as the sling (swing seat ) allows. In addition, when the urethra is pushed against the sling it will be compressed shut which helps in people who have scarred, brittle urethra walls from prior surgery (a condition called ISD).
Most slings today are made of Prolene mesh which is the same material as fishing line. It is nonreactive (your body ignores it), permanent and has a long track record of use in female pelvic surgery. These slings can be done as an out patient and you can be back to work in a matter of a couple of days. Restrictions are minimal and you can resume all activities in three weeks. Biological tissue can also be used. The most common is fascia which is the fibrous band running down the outside of thigh. This can either be taken from your body or obtained from a tissue bank. Recovery from a biological sling includes restricted activities for six weeks to allow for proper healing. An example of someone who would need a biological sling is a patient who has had radiation therapy for cervical or vaginal cancer because of an increased chance of the manmade sling eroding through the tissues. For a review of stress incontinence and sling surgery click here.
In some cases the urethra walls can be bulked up by injecting agents such as collagen (yes the same material the stars use in their lips), or graphite particles into the walls to get a tighter closure. Various materials are being researched but the perfect agent is not available as of yet. The upside of these procedures is that they can be done in the office. The downside is that they are not permanent and have to be repeated periodically.